Reframing Hormone Therapy for Women: The Science of Estrogen, Progesterone, and Long-Term Vitality
By Kevin Cooke, MD — Board Certified in Family Medicine and Performance Medicine
Introduction
For decades, the conversation around hormone therapy in women was clouded by fear and misinformation. The Women’s Health Initiative (WHI) study in 2002 led to widespread panic about estrogen therapy, dramatically reducing its use. But what was missed in that narrative is crucial: the original study population was older, many years past menopause, and most received oral conjugated equine estrogens with a synthetic progestin—not the bioidentical hormones we use today.
Since then, a wealth of evidence has clarified that timing, formulation, and delivery are everything. For many women, hormone replacement therapy (HRT) — when started at the right time and monitored precisely — can significantly improve quality of life, cognitive performance, and long-term health outcomes.
This isn’t about “anti-aging.” It’s about restoring the hormonal signaling that protects the brain, heart, and bones during the critical decades after menopause.
The Hormonal Symphony: Estrogen and Progesterone
| Hormone | Key Roles | What Declines Cause |
|---|---|---|
| Estrogen (Estradiol) | Maintains bone density, vascular health, insulin sensitivity, and neuronal growth | Hot flashes, night sweats, anxiety, memory issues, bone loss, metabolic slowdown |
| Progesterone | Calms the brain via GABA receptors, stabilizes mood, protects the endometrium | Sleep disturbance, anxiety, irregular bleeding, mood instability |
| Testosterone (in smaller amounts) | Contributes to libido, energy, and muscle tone | Fatigue, loss of motivation, lower sexual desire |
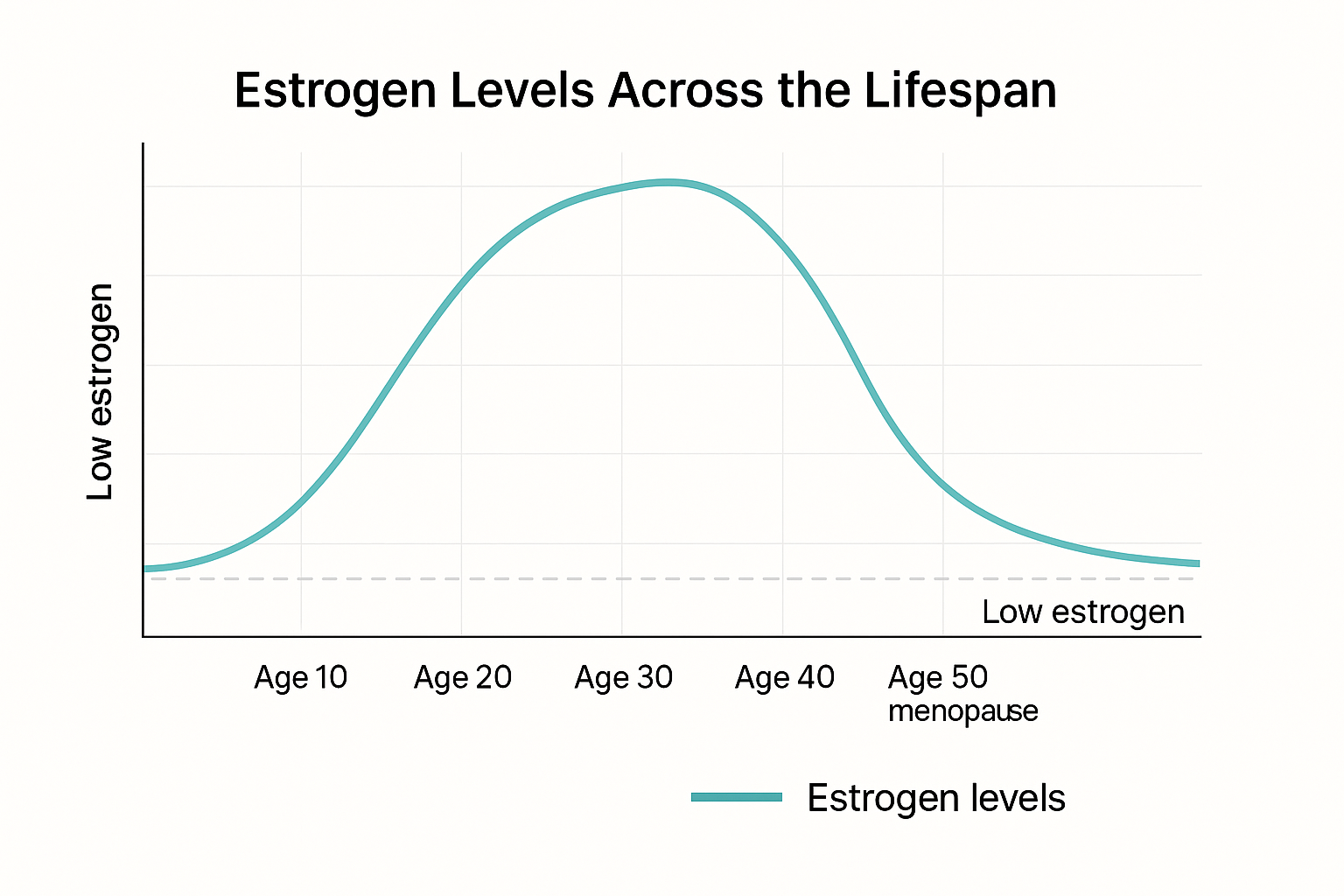
Menopause is not just the cessation of menses — it’s a neuroendocrine transition that affects every system: from mitochondria to neurotransmitters. Estrogen receptors are found in the brain, heart, bones, skin, and gut, meaning the decline is systemic.
The Estrogen Window: Why Timing Matters
Dr. Peter Attia frequently emphasizes the “timing hypothesis” — the concept that estrogen’s benefits depend heavily on when therapy begins.
Women who start HRT within 10 years of menopause onset — ideally between ages 45 and 60 — show lower all-cause mortality, reduced coronary artery calcification, and better cognitive outcomes compared to those who begin later.
| Timing of Initiation | Cardiovascular Risk | Cognitive Outcomes |
|---|---|---|
| Within 10 years of menopause | Decreased risk of CHD and all-cause mortality | Preserved memory and attention |
| More than 10 years after menopause | Increased risk if plaque is already present | Higher risk of dementia |
Data from The Kronos Early Estrogen Prevention Study (KEEPS) and ELITE Trial.
The Brain Connection
Andrew Huberman has described how estrogen acts not just as a reproductive hormone but as a neuromodulator — influencing serotonin, dopamine, and acetylcholine signaling. These neurotransmitters govern motivation, sleep, learning, and emotional regulation.
Loss of estrogen decreases synaptic density in the hippocampus and prefrontal cortex — regions critical for memory and focus. That’s why many women describe “brain fog” or feeling “not like myself” as their first symptom of menopause.
Interestingly, brain imaging studies have shown that women who initiate transdermal estradiol during early menopause have better preservation of gray matter volume and lower amyloid accumulation — potential markers of Alzheimer’s protection.
What the Modern Evidence Says
When bioidentical hormones are used — 17β-estradiol (topical or transdermal) combined with micronized progesterone— the risk-benefit profile changes dramatically.
| Outcome | Effect of Bioidentical HRT | Evidence Source |
|---|---|---|
| Hot flashes, night sweats | Major reduction in frequency & severity | WHI follow-up, KEEPS, ELITE |
| Sleep quality | Improved deep sleep and REM | Randomized trials, JAMA 2020 |
| Cognitive function | Slower decline in verbal memory and processing | Mayo Clinic, 2021 cohort |
| Bone health | 30–50% reduction in hip fracture risk | NEJM, 2018 |
| Cardiovascular disease | Reduced atherosclerosis progression if started early | ELITE Trial, 2016 |
| Breast cancer risk | Neutral to reduced with transdermal estradiol + progesterone | French E3N Cohort (80,000+ women) |
French E3N Cohort (over 80,000 women)
Delivery Matters: Oral vs. Transdermal
Route of administration is not cosmetic — it’s biology.
Oral estrogens undergo first-pass metabolism in the liver, increasing clotting factors and triglycerides.
Transdermal estrogens (patches, gels, creams) bypass the liver and maintain a more physiologic estradiol-to-estrone ratio, reducing the risk of thrombosis and stroke.
Similarly, micronized progesterone (bioidentical) supports natural GABA activity in the brain — improving sleep and calm — whereas synthetic progestins (like medroxyprogesterone) blunt these effects and raise cardiovascular risk.
The goal is to restore physiology, not override it.
The Whole-System Approach
Hormones don’t exist in isolation. Optimizing estrogen and progesterone works best when integrated into a broader performance and longevity framework:
| System | Target | Supporting Strategy |
|---|---|---|
| Metabolic | Improve insulin sensitivity | Protein 1.6–2.0 g/kg, resistance training, time-restricted eating |
| Neurocognitive | Preserve gray matter, reduce inflammation | Sleep 7–8 hrs, omega-3s, mindfulness, aerobic exercise |
| Skeletal | Maintain bone density | Strength training, vitamin D + K2, adequate calcium |
| Cardiovascular | Reduce plaque risk | Transdermal estradiol, ApoB <80, optimize blood pressure |
| Mood & Sleep | Enhance GABA and serotonin tone | Micronized progesterone at bedtime, circadian light exposure |
Hormone therapy amplifies the signals your lifestyle sends. If those signals are poor — poor sleep, high stress, poor diet — you’re amplifying dysfunction. The most powerful results come when biology and behavior are aligned.
Monitoring and Safety
Responsible HRT always involves monitoring.
Initial evaluation includes:
Estradiol (E2)
Progesterone
FSH, LH
SHBG
Lipid panel, ApoB
Hematocrit
Liver function
Follow-ups are typically every 3–6 months, with adjustments based on both labs and symptoms. The goal is not a number — it’s a physiologic balance.
The Takeaway
| Principle | Summary |
|---|---|
| Timing is everything | The “estrogen window” matters. Early initiation = protection. |
| Formulation and delivery matter | Bioidentical, transdermal estradiol + micronized progesterone are safest. |
| Lifestyle synergy | Sleep, strength, and nutrition determine therapy success. |
| Monitor intelligently | Track labs, symptoms, and long-term metrics like ApoB and bone density. |
| Goal: Restore, not boost | The aim is balanced physiology, not supraphysiologic levels. |
References
Hodis HN et al. ELITE Trial. NEJM, 2016.
Harman SM et al. KEEPS Trial. Ann Intern Med, 2014.
Fournier A et al. E3N Cohort Study. BMJ, 2008.
Santoro N, Pinkerton JV. Menopause, 2020.
Attia P. The Drive Podcast: Hormone Optimization in Women, Episodes #204, #217.
Huberman A. Huberman Lab Podcast: Hormones and the Brain, 2023.
Closing Thoughts
Hormone therapy, done right, isn’t about reversing age — it’s about preserving vitality. Estrogen and progesterone are not optional; they are regulatory systems for nearly every cell in the body.
When replaced with precision and monitored over time, they help women remain strong, clear-minded, and metabolically resilient through the decades when chronic disease risk begins to rise.
If you’d like to explore whether HRT is right for you, our practice offers comprehensive hormone and metabolic testing, along with tailored lifestyle and nutrition strategies to support healthy longevity.